Unlocking Cognitive Potential in Special Needs Children Through Occupational Therapy
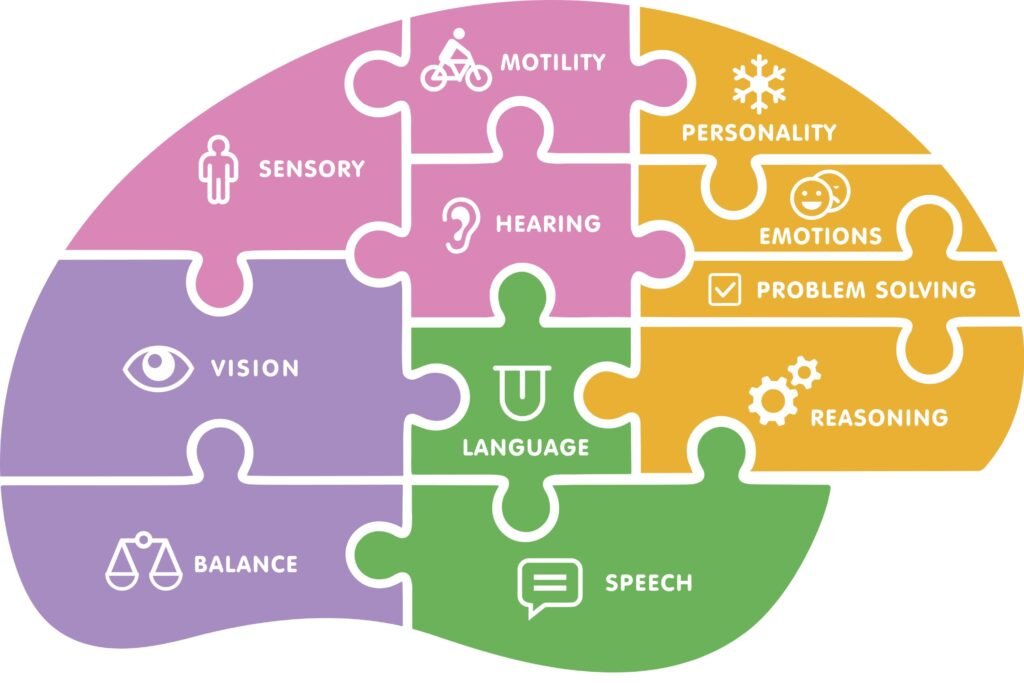
Unlocking Cognitive Potential in Special Needs Children Through Occupational Therapy Uncategorized February 12, 2025 Cognitive development plays a crucial role in a child’s overall growth and well-being, especially for those with special needs. Many children with conditions such as autism, ADHD, cerebral palsy, or other developmental disorders may experience challenges in cognitive and motor skills that impact their daily lives. Fortunately, occupational therapy offers a powerful tool to unlock a child’s cognitive potential, helping them build the skills they need to succeed both in and outside the classroom. In this article, we’ll explore how occupational therapy for special needs children can play a transformative role in supporting cognitive development for children with special needs and improving their ability to engage with the world around them. What is Occupational Therapy for Special Needs Children? Occupational therapy for special needs children is a healthcare profession that focuses on helping individuals develop, recover, or maintain the skills needed for daily activities, known as “occupations.” For children with special needs, these occupations can include tasks like eating, dressing, writing, playing, or interacting with peers. An occupational therapist (OT) works with children to assess their abilities, develop personalized treatment plans, and provide interventions that target specific cognitive skills, motor skills, and sensory challenges. In children with special needs, occupational therapy addresses both fine motor skills (like holding a pencil, using scissors, or manipulating small objects) and cognitive skills (such as attention, memory, problem-solving, and executive functioning). The ultimate goal is to promote independence, confidence, and success in various aspects of life. How Occupational Therapy Enhances Cognitive Development Occupational therapy offers several strategies that can help unlock cognitive potential in children with special needs. Here are some of the key ways OT supports cognitive development in children with special needs: Improving Attention and Focus Children with special needs often struggle with attention and focus, which can hinder their learning and social interactions. Occupational therapy for cognitive development includes activities that help children enhance their ability to stay focused on tasks and improve their attention span. Techniques might include: Structured routines: Creating consistent daily schedules to help children anticipate what’s next and reduce distractions. Sensory integration techniques: Using activities that stimulate or calm the senses to help children regulate their focus and emotions. Task breakdowns: Breaking tasks into smaller, manageable steps to make them less overwhelming and easier to follow. Developing Problem-Solving Skills Children with special needs may struggle with understanding and solving problems in everyday situations. Occupational therapy helps build problem-solving skills by providing opportunities to engage in activities that require thinking through steps, overcoming obstacles, and making decisions. Examples include: Puzzles and games: Encouraging children to engage with problem-solving tasks such as puzzles, building blocks, or simple games that require strategy. Sequencing exercises: Working on activities that involve sequencing (such as following a set of instructions or arranging objects in order) to boost cognitive organization and logical thinking. Building Executive Functioning Skills Executive functions are the mental processes that allow children to plan, organize, and execute tasks. These skills are vital for academic success and independence. Occupational therapy can target areas of executive functioning like: Organization: Helping children organize their materials, tasks, and environments, improving their ability to complete tasks efficiently. Time management: Teaching children how to manage their time through scheduling, planning, and prioritizing tasks. Self-regulation: Helping children manage emotions and behavior, enabling them to focus and stay on task. Enhancing Sensory Processing Many children with special needs experience sensory processing challenges, which can affect how they respond to sensory stimuli like light, sound, textures, or touch. These sensory challenges can impact cognitive development and daily functioning. Through sensory integration therapy, occupational therapists help children process and respond to sensory input more effectively by: Gradual exposure: Gently introducing sensory experiences in a controlled way to help children build tolerance and adaptability. Calming techniques: Teaching children strategies like deep breathing, swinging, or sensory-friendly tools to help them regulate their sensory input and stay calm. Sensory-rich activities: Using textures, colors, and sounds in therapy sessions to help children engage with and process sensory information. Improving Social Skills Cognitive development isn’t just about individual tasks; it’s also about how children interact with the world and others. For children with special needs, occupational therapy often includes activities that help with social cognition—the skills needed to understand social cues, communicate effectively, and build relationships. Techniques include: Role-playing: Practicing social scenarios with a therapist or peers to build confidence in social interactions. Group activities: Engaging children in group tasks to help them learn to collaborate, share, and communicate with others. Fine Motor Skills and Hand-Eye Coordination While not directly linked to cognition, fine motor skills such as writing, cutting, and manipulating small objects are crucial for a child’s academic and cognitive progress. By improving these skills, occupational therapy helps children engage in more complex cognitive tasks, such as reading and problem-solving. When Should You Seek Occupational Therapy for Your Child? If your child has special needs and is experiencing difficulties with cognitive development, occupational therapy can provide valuable support. It’s important to seek professional help if your child is: Struggling with attention, focus, or following directions. Having trouble with tasks like writing, drawing, or using utensils. Facing challenges in processing sensory information. Showing signs of poor social skills or difficulty interacting with peers. Having difficulty with self-regulation or managing emotions. An occupational therapist can assess your child’s needs and develop a personalized treatment plan to address these challenges, ultimately enhancing your child’s cognitive development and overall well-being. Conclusion Occupational therapy plays a key role in unlocking the cognitive potential of children with special needs. By targeting critical areas such as attention, problem-solving, executive functioning, sensory processing, and social skills, occupational therapy provides children with the tools they need to succeed in everyday tasks and thrive in their academic and social environments. With the right support, children with special needs can build the cognitive and life skills that set them on a path to greater independence and success. If you believe your child could benefit from occupational therapy, don’t hesitate to contact Budding Blossom Paediatric Rehab Centre. Our experienced therapists can assess your child’s needs and develop a tailored treatment plan to support their cognitive development and growth.